Open the door to a New Life with...
Learn About The RESTORE Ultra-Rapid Infusion Difference...
Restore | Reboot | Recover...with RESTORE

The RESTORE Ultra-Rapid Infusion Difference
Our Clinical Findings Have Been Presented Internationally

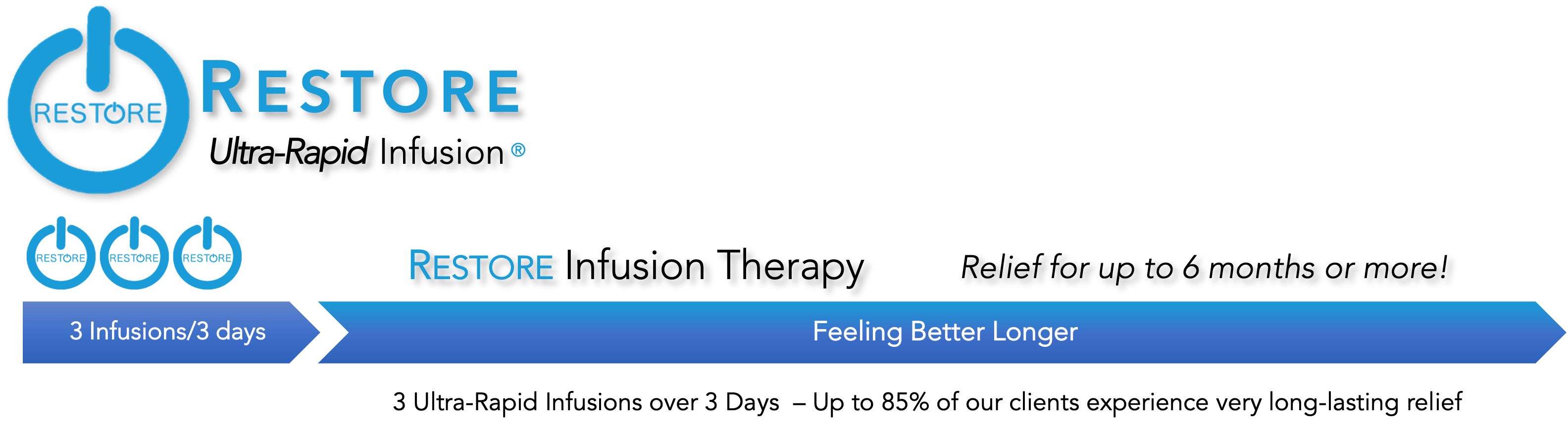
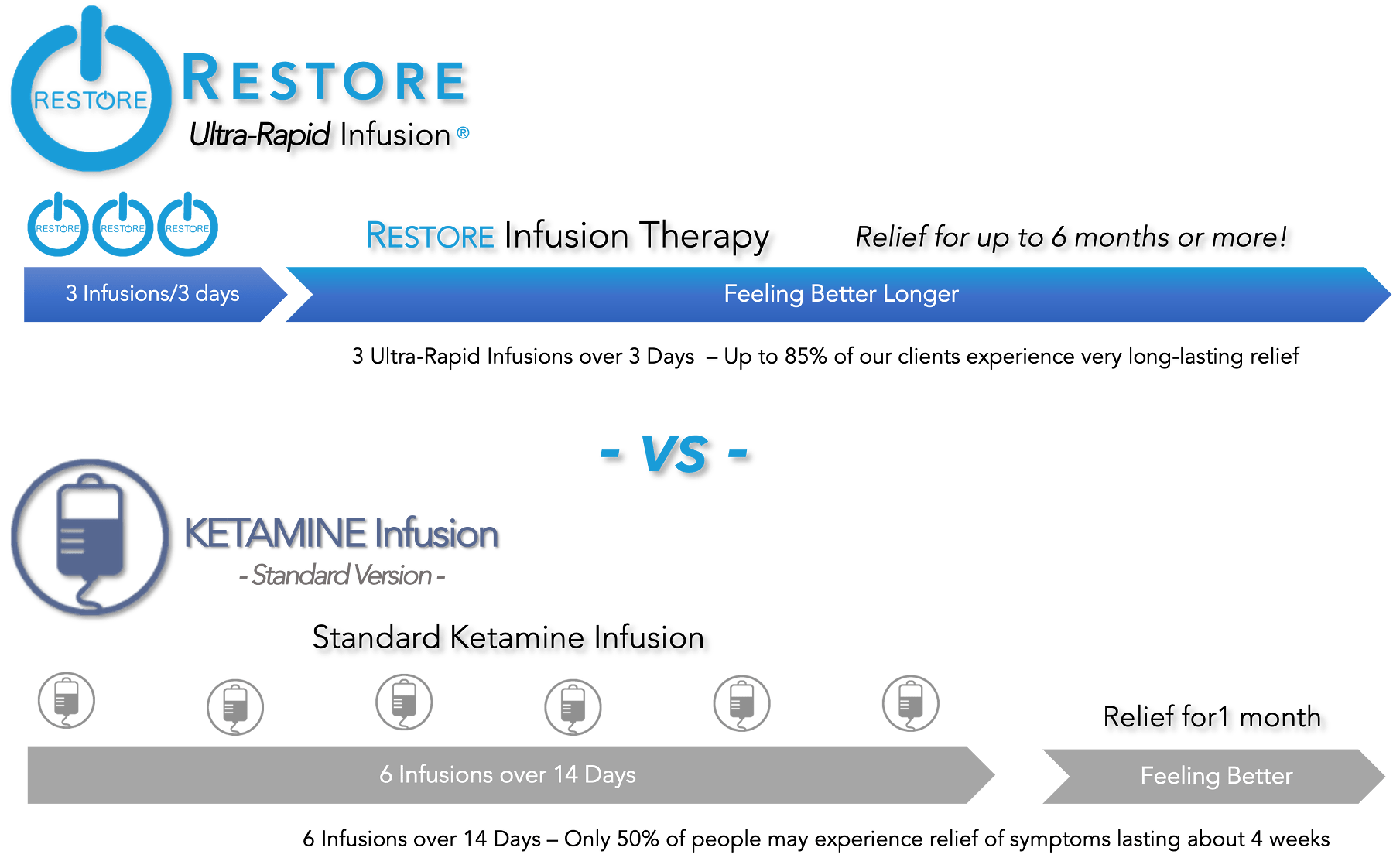
The RESTORE Ultra-Rapid Infusions are uniquely different from the "standard ketamine infusion" developed years ago. It is the most advanced formulation of therapy available and is not only more effective than the "standard" ketamine infusion; but when enhanced with our unique protocol it can last 3-6 times longer and need fewer "booster" infusions than standard ketamine infusions do. And the beneficial results can begin in just minutes to hours after the first infusion.
If you’ve suffered for years and given up hope of ever finding relief, then the RESTORE Ultra-Rapid Infusion program can almost sound too good to be true. But the number of patients receiving this revolutionary new therapy is growing rapidly. Today, almost 20 years after the breakthrough discovery at Yale, the next generation of ketamine therapy - the RESTORE Ultra-Rapid Infusion - is finally starting to reach the patients who need it most.
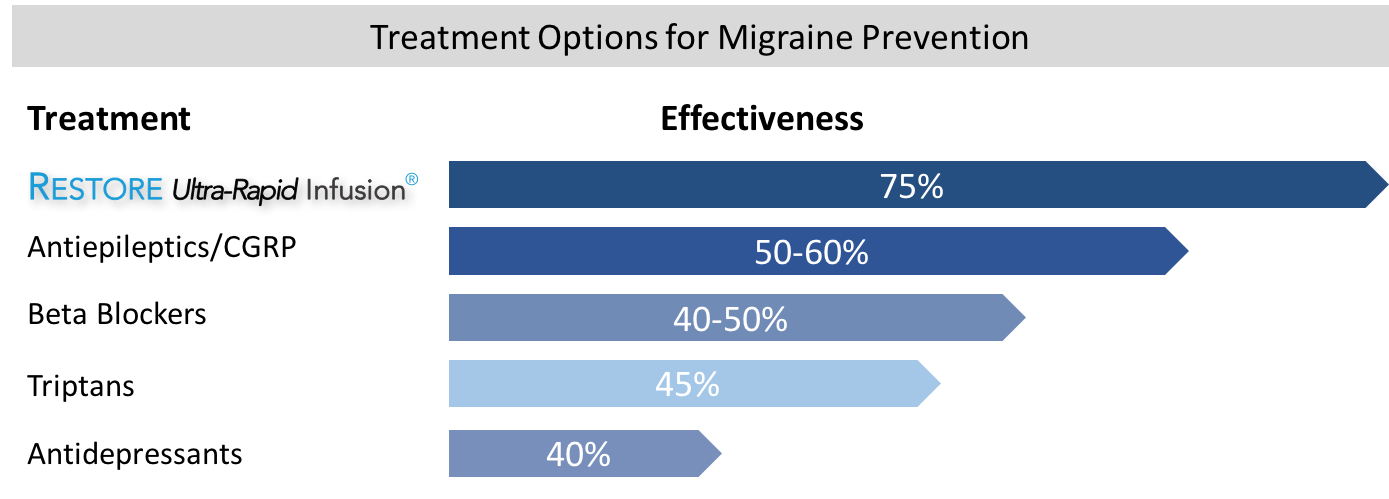
We understand that living with Chronic Neuropathic Pain, Migraines, Fibromyalgia, and Depression can be difficult, but considering RESTORE Infusion Therapy is a step in the right direction. Choosing RESTORE is a decision you and your doctor make together. And you’re not alone. RESTORE Ultra-Rapid Infusion therapy has been used to treat hundreds of patients all across the country and internationally.

Why RESTORE Ultra-Rapid Is So Effective
It's All About The "Disconnected" Brain

There Is A Reason Why Current Medications Don't Work Well.
If your current prescription medications are falling short, recent discoveries in brain imaging studies reveal a new treatment and why it might help.
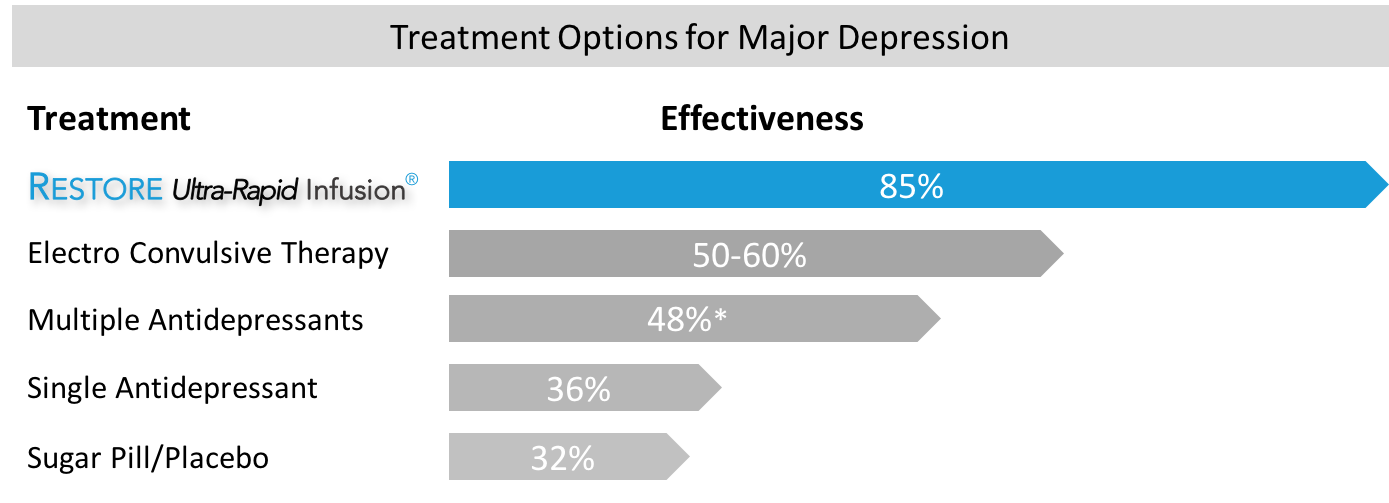
Medications are a standard and sometimes an effective treatment for depression, migraines, and Fibromyalgia, but they are far from perfect. In fact, in some cases, our current medications have proven to be no better than a sugar pill or placebo, and some patients don't respond to any of the drug options currently available.
I've Tried Everything And... Nothing Works!
Even after over 50 years of medical research, prescription medications have not been very effective in treating most people suffering from depression, migraines, Fibromyalgia, and other forms of chronic pain. These limited treatment options represent a vast clinical challenge, and many people continue to struggle.
From the time drugs were first developed back in the 1950s to today, they have all worked through similar biochemical actions. The most commonly known and prescribed class of drugs is the selective serotonin reuptake inhibitor, or "SSRI." These drugs, including the brands Prozac, Zoloft, Paxil, and Lexapro, attempt to regulate the amount of serotonin, a brain chemical called a neurotransmitter that carries signals between neurons and thought to control mood. The assumption is that if you could increase the amount of serotonin (or dopamine or norepinephrine) available, your symptoms would improve.
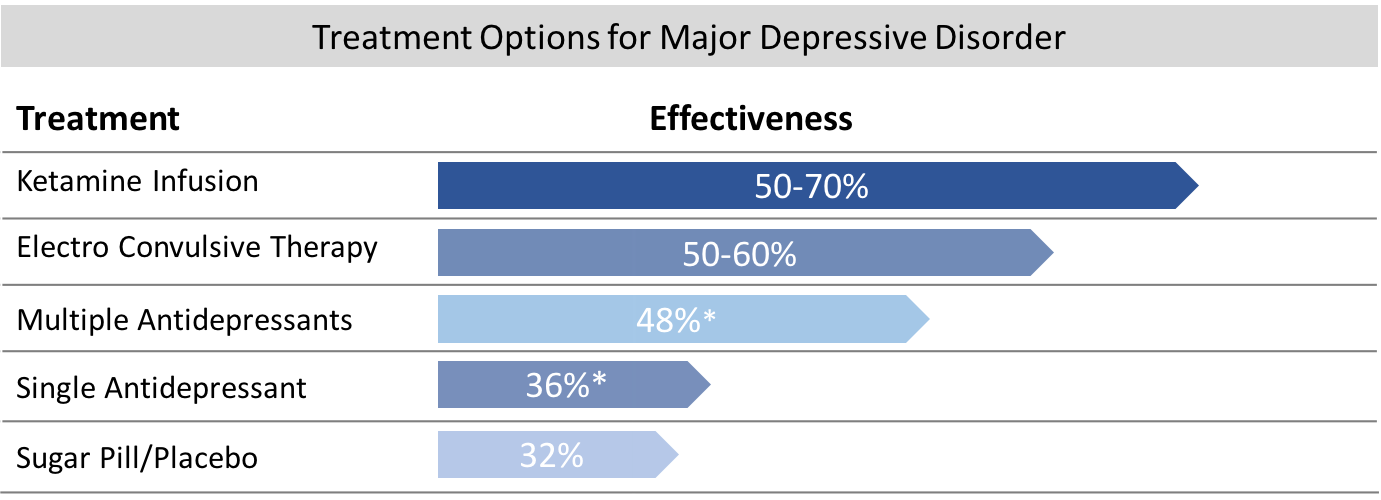
Unfortunately, they have not been as helpful as we had hoped for many people. And the rate of response to them is not as high as we need it to be. Studies have shown that only 1 in 3 patients respond to any single SSRI. And if they do respond, it can take several weeks or months before experiencing improvement. Even more aggressive new treatments to combat mood disorders such as transcranial magnetic stimulation (rTMS) are only about 38% effective, and even the older "gold standard" treatment of psychiatry, electroconvulsive shock treatment (ECT), is not much better. It is only effective for about 50% of patients.
Why Haven't We Been Able To Do Better?
Until now, treatments for depression with antidepressants assumed that low levels of brain neurotransmitters like serotonin and dopamine were the cause of depression. But what if we were wrong? The answer to that question may be becoming apparent with new cutting-edge research and brain imaging studies showing how the brain works.
Significant findings emerged in the late 1990s with the observation by researchers that brain tissue in critical areas of the brain was reduced in people who had been under prolonged stress and in combat veterans who had developed depression and PTSD.
Investigators at Stanford University suggested that stress might cause the "death" of neurons, suggesting that the critical brain size reductions seen in patients under stress and those with depression and PTSD might reflect the loss of nerve cells.
These new findings suggest that the old theory about low serotonin causing these illnesses may be incorrect. But why were these vital areas of the brain "shrinking" and getting smaller and smaller?
The "Disconnected" Brain
The answer to that question was found with the development of a new way type of MRI study called Diffusion Tensor Imaging or "DTI." Using DTI techniques, researchers could examine these areas and the "neural network connections" around them in much greater detail.
With this new way of looking at the brain's inner workings, it became apparent that these critical neural circuits, which play an essential role in the development of major depressive disorders, Fibromyalgia, and even migraine headaches, were becoming "disconnected" and isolated in some way.
They saw microscopic changes occurring between the white matter (wiring-neural circuit pathways) of the higher and deeper layer of the brain known as the cortical-subcortical circuits, leading to a type of "disconnection syndrome" between those regions. This decrease in "connectivity" linking the various critical areas of the brain appears to be directly involved in developing multiple disorders, including depression, anxiety, and PTSD.
The loss of these connections means that various areas of the brain may no longer communicate information effectively and become stuck in a sort of continuous "loop." Almost like a computer program that freezes and won't work correctly. It now appears that this "disconnection" in the brain's wiring network and loss of communication is responsible for low neurotransmitter levels.
The repetitive circuits may only communicate limited signals, like continuous thoughts and feelings of depression, anxiety, or pain, by losing those connections. We now suspect that as these critical connections are lost or "disconnected," people may feel depressed, and anxious, or start to experience pain, increased sensitivity, and headaches. Often, they also report having difficulty concentrating or remembering important information. The result is that everyday life can become challenging and less meaningful. Friends, family, and things they used to enjoy no longer seem to please them.
It can seem almost as if someone has slowly and methodically "turned off" all the light switches in a big house, and now the house becomes cold, uncomfortable, dark, and gloomy.
If that is the case, the question then becomes: can you restore those lost connections?
New Options to "Reboot and Reconnect" the Brain
New research shows additional evidence supporting the "disconnection syndrome" theory and suggests that the connections can be "restored or rebooted."
Part of that research was the discovery that a 50-year-old medication commonly used for anesthesia can have some very remarkable "side effects." Researchers were astonished when they discovered that following the intravenous administration of ketamine, they saw a rapid "reconnection" of the brain network. More than that, they found that following the treatment, brand new nerve connections began to develop almost immediately.

Ketamine was found to have this unusual effect by stimulating a brain "nerve growth" factor known as BDNF, which could reverse some of the disconnections in minutes. That small study conducted at Yale also established an arbitrary "standard" for ketamine infusions in the treatment of mood disorders. The standard was, and is, to this day - "administer 0.5mg/kg of ketamine over 40 minutes" based on body weight.
While the effects of ketamine were astounding, and it was truly remarkable that the brain could be "reconnected" so quickly, there was a catch. After a single infusion, the "rebooting" only lasted 3-7 days before the connections were lost and symptoms returned.
How could it be made to last longer?
The Standard Medical Model -
How Others Tried To Make Ketamine Last Longer
The Old ECT Model
 To study this, one group in Minnesota and another in New York thought that ketamine might work like another older and more aggressive form of therapy known as electroconvulsive therapy or "ECT." They knew that it usually requires six or more ECT sessions before a person improves, so perhaps ketamine needed to be given more than once, just like ECT.
To study this, one group in Minnesota and another in New York thought that ketamine might work like another older and more aggressive form of therapy known as electroconvulsive therapy or "ECT." They knew that it usually requires six or more ECT sessions before a person improves, so perhaps ketamine needed to be given more than once, just like ECT.
To test this hypothesis, they began to administer six ketamine infusions, one every other day for two weeks, just like they would for ECT. What they found by doing that was that the improvement seen could be extended to 1 month before the patients needed another infusion. That was better than 3-7 days, but patients continued to need ongoing "booster infusions" every four weeks after that to make it last.
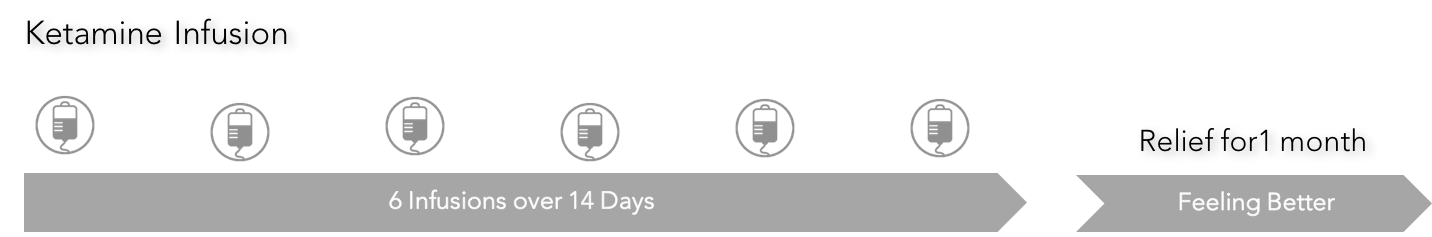
While six infusions given every other day for two weeks did improve the benefits of ketamine substantially, many patients found it challenging to return each month for "boosters." We thought it could be better, and it was always a little surprising that few have had the imagination, experience, or expertise administering ketamine infusions to improve on it.
Since then, others have adopted that same protocol without realizing or understanding that it was not intended to treat depression, nor was it ever optimized to achieve the most effective serum concentrations necessary. So, today, the only factor that many physicians and "ketamine clinics" consider when determining your infusion is your body weight. They rely upon a simple, straightforward formula of "so many milligrams" of ketamine per kilogram of your weight and administer the infusion over 40 minutes.
Using that approach, the results today are about the same as they were almost 20 years ago. Approximately 70% of research-study patients will show improvement, while only about 40-50%. of "real-world" patients who are treated in a community ketamine practice will have a 50% or better reduction in their symptoms for about one month before requiring another infusion to maintain the benefits. Still, even with the need for six infusions to have the effects last one month, the effectiveness of this approach is far better than those obtained for many with conventional antidepressant therapy.
Although I was initially impressed with the results, it was also clear that many other factors could influence how well the infusion worked. After all, we all have taken either over-the-counter or prescription medications at one time or another, and most medications come in various strengths for different conditions. For example, Prozac, an older and very common antidepressant, is supplied in 10mg, 20mg, 40mg, 90mg strengths. It is available that way because each person will metabolize the drug differently, some more slowly and others very rapidly, leading to different amounts of the medication in their system. Some conditions may be more challenging to treat and require more medicine to be effective. Also, there may be potential drug interactions to consider. Whenever we start a new medication, our practitioner or pharmacist will also warn us about taking other medicines simultaneously and how they might negatively interact. The same is also true for ketamine.
So, just based on common sense and logic, there was room for improvement with ketamine infusions utilizing the same approach. The first step was to determine if other doses or specific serum concentrations of ketamine would be more effective or last longer. Once that was determined, the next step was to determine the time necessary to maintain that concentration for each person to have a maximal effect. Finally, what other metabolic or medication issues affect how well someone would respond or how long the improvements would last?
We took a different approach...
 Precision Medicine -
Precision Medicine -
New Solutions Require New Ways Of Thinking
The New RESTORE Ultra-Rapid Approach
We knew we had to look at this in a new way to get the best results, so we took a different approach. Some people have the impression that all people with an illness like depression, Fibromyalgia, or migraines are alike. With that thinking, you give the same medication, in the same amount, to everyone in the same way and hope they improve. Unfortunately, as we all know, it doesn't always work well that way.
But we knew that each person is unique and different, so it was apparent that the treatment must be individually tailored to match the patient. Rather than use an old model like ECT, we used a new integrated and systems model. Using the same old methods and expecting different results never leads to breakthroughs.
There were many factors to consider. First, the medication needed from patient to patient can vary greatly. Based on our experience, we knew that it was critically important to achieve a certain "blood level" or effective serum concentration, also known as the effective dose for 95% of patients or (ED95), to achieve optimal results. This can be challenging, and many physicians are unaware of the optimal serum concentrations needed.
But there was even more than that to consider. Precision Medicine and innovative clinical research have shown a wide variation in the way people metabolize medications, which is often due to liver enzymes known as Cytochrome P450. More than that, some individuals may lack acetyl-L-carnitine (LAC) or have a BDNF variant, which may affect optimal treatment response. It is also vital to account for other factors such as current medications, metabolism, body composition, ancestral heritage, and genetic factors, which all play a critical role in treatment response. All of these factors need to be considered to have the best result.
And then, we found that it was not only essential to optimize the amount of medication given, but we had to change the way it was administered. It had to be carefully adjusted to each patient, minute-by-minute, while constantly monitoring them and adding synergistic agents; if all of that was done very carefully, then ketamine worked remarkably better and lasted much longer. Following this approach, we discovered we could achieve better results with only three infusions and that they would last for 3-6 months.
Over a 7-year period, I was able to identify and determine what those optimal levels were, the time necessary to maintain them, and what effect body metabolism and other medications had on the infusion. For example, to have predictable and consistent results, body mass composition, not total body weight, directly affects the serum concentration of ketamine achieved during an infusion. Also, I found that a person's basic metabolic rate for drugs, current medications, hormones, and carnitine levels all affect the response to ketamine. So, before we consider beginning an infusion, we spend a great deal of time determining if each patient is in an optimal state to have an infusion or requires specific additional lab tests or supplementation before beginning infusion therapy to have the best results.
In addition to metabolic optimization before therapy, the RESTORE infusion it self is unique in significant ways. RESTORE utilizes a combination of ketamine combined with magnesium additives to make it more effective than ketamine alone. Magnesium acts as a synergistic agent, or cofactor, which works at the same NMDA receptor sites as ketamine does and is necessary for an optimal response. However, it must be given at the correct time and in the correct ratio to have a maximal effect when provided in this way; it can increase the responsiveness of NMDA receptor to ketamine by 2-3 times.
Not stopping there, we have also employed additional neuromodulators to significantly increase the effectiveness of ketamine. Specific well-known molecules can augment the binding affinity of ketamine for its receptor targets. At the same time, others can enhance the downstream effects of BDNF and mTOR activation, which promote neurogenesis and synaptic plasticity. The addition of these “ketamine-promoters” can unlock the full potential of ketamine’s therapeutic effect.
Most importantly, the older infusion protocol has also been improved to a more sophisticated 3-stage variable rate infusion. Utilizing this approach, RESTORE achieves optimal blood levels much faster and maintains them for a more extended period of time. By optimizing serum concentrations in this way, the RESTORE infusion program achieves higher effective serum concentrations of the parent molecule ketamine and higher concentrations of the critical secondary metabolites of ketamine known as HNK (Hydroxynorketamine) and DHNK (Dehydronorketamine). This is important because it is the secondary metabolites of ketamine that promote the long-term benefit by increasing BDNF (brain-derived neurotrophic factor) levels over a more prolonged time. Increased levels of BDNF have been found to contribute to the enhanced neuroplasticity and synaptic connectively seen with ketamine.
We have also found that post-infusion supplementation with those same and additional cofactors in a specific ratio promotes and enhances the infusion benefits and increases how long it lasts. All of this, of course, does not speak to the possible therapeutic benefits that can occur from the psychological experience achieved during an infusion. By optimizing the serum concentrations in the way we do, each person has the best opportunity to gain personal insights, understanding, and a new perspective that can sometimes greatly aid in the recovery process.
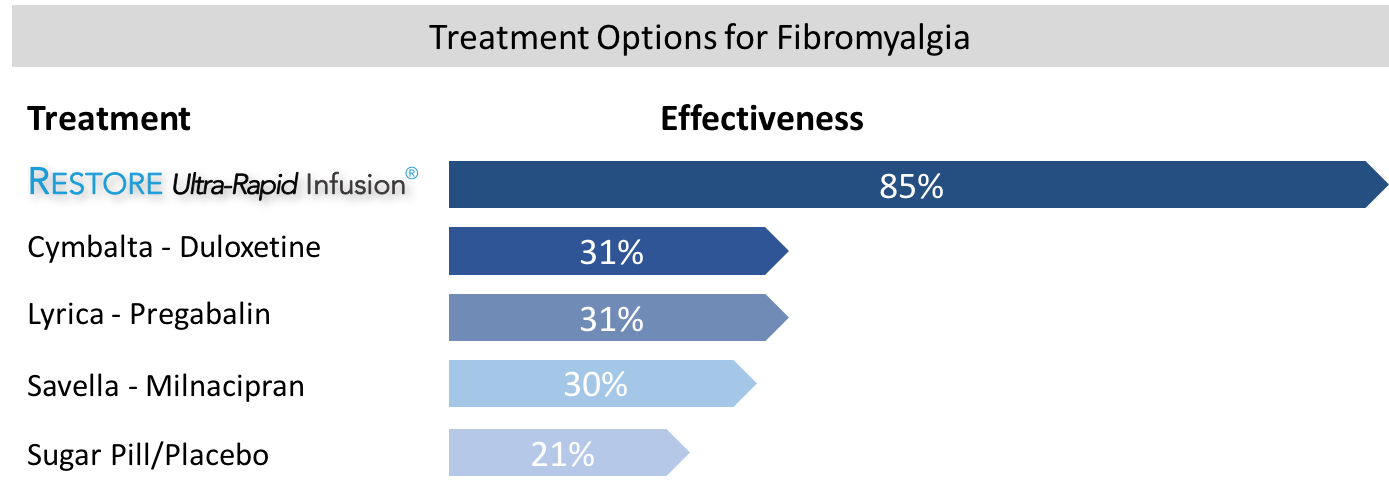
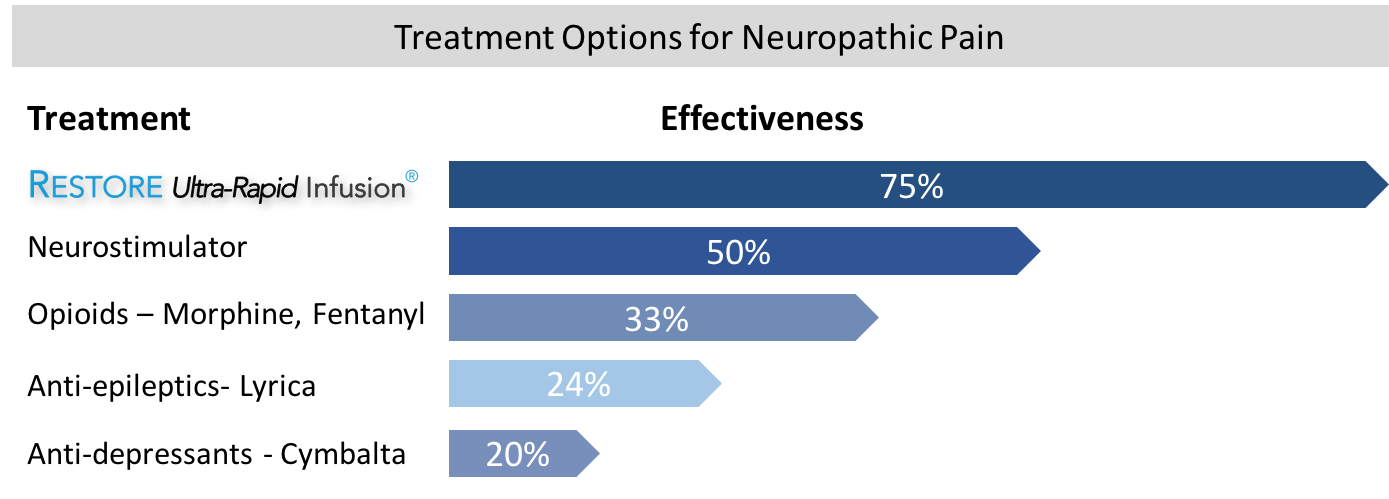
Although the RESTORE infusion program is much more involved and complex than a conventional ketamine infusion, the results, at least in our opinion, are worth it. RESTORE has a broader range of disorders that can be treated successfully, and it is more effective (85% vs. 70%), more efficient (3 treatments vs. 6 infusions), and longer-lasting (3-6 months vs. 1 month) than conventional ketamine infusions. Lastly, it is also less expensive and more cost-effective compared to a ketamine infusion.
Using this new "RESTORE" model and treatment protocol, we have had outstanding results in people who didn't respond to any medication, therapy, magnetic stimulation, ECT, or even the "old ECT model of ketamine administration." The RESTORE Ultra-Rapid Infusion is the result of years of hard work. It is an advanced treatment that can significantly enhance and restore brain connectivity, and is capable of establishing new neuronal connections within minutes of treatment.
You Can See The Results...
See The RESTORE Difference For Yourself
Depression
Migraine Headaches
Fibromyalgia
Neuropathic Pain - Including CRPS/RSD
What The Future May Hold...
The future of drug treatment for migraines, fibromyalgia, and depression, as with many other diseases, lies in the genetic code and a better understanding of how the disorder occurs. Realizing the tremendous potential of ketamine therapy, numerous pharmaceutical companies are developing other versions of ketamine that can be given in different ways, including as an oral medication or a nasal mist.
Major drug companies, including Johnson & Johnson, Janssen, and Allergan are stopping research into older antidepressants and rushing into the development of new drugs that they hope will come close to duplicating the rapid and remarkable benefits of the ketamine infusion.
There is little wonder why this happens when you consider the dramatic improvements that can occur in just 24 hours after a single infusion. No current medications or treatments that can match the seen with ketamine. While the pharmaceutical companies are trying to make something almost as good as ketamine, the results have been disappointing.
We have taken another path...
Rather than changing what we already know works well…we made it even better and longer-lasting!
It may be a few years before any of these other ketamine-like treatments or other drugs are FDA-approved. Nonetheless, because the drug is already approved for other uses, some physicians are recommending RESTORE Ultra-Rapid Infusion therapy for their patients with migraines, fibromyalgia or treatment-resistant depression now.

That is the RESTORE Ultra-Rapid Infusion Difference.
The Ketamine Research Institute and the RESTORE Infusion Center — Known Worldwide

If you suffer from chronic pain or depression and have not had relief with prescription medication or other traditional treatment modalities, then the RESTORE Ultra-Rapid Infusion therapy program may be an option for you. We will be happy to provide you with an initial consultation to see if infusion therapy is right for you.
Just call us today:
800.850.6979
“The most important breakthrough in antidepressant treatment in decades”....
Thomas Insel, MD - Director, National Institute of Mental Health





