The fact is...
“some of the most significant research occurs at the interfaces between traditional research areas. This is even more likely to be true in the future because the solution to complex biological and health care problems require experts and expertise in many different disciplines—and increasingly expertise in more than one field.”
Let's Look At This A New Way.
RESTORE Infusion Development
When research scientists try to discover a new drug or molecule to treat an illness, like pain or depression, they approach it from what they believe is a very practical and standardized way. They have identified a problem in need of a solution, in this case chronic pain and depression, so they then try to find a new molecule, or a modification of an old one, that will correct it. This can take years of research with trial and error investigation to attempt to find the “magic bullet” cure.
That’s the standard, traditional approach. But what happened with Ketamine was very different. Ketamine is a drug that has already been around for 50 years and it was “accidentally discovered” that it could treat pain and depression far better than anything we currently have available. How could that be?...How does it work?
![]()
Now the research is focused on trying to break it down “receptor by receptor” and “protein by protein” to find out how it does this. While this will be valuable information to have, it will take many more years of research and likely not add a great deal more value than we realize now….it works!
We have taken a different approach. We already know ketamine works, but if used by itself, it has several short comings…. so rather than "breaking it down" we have chosen to pursue ways to “build it up” correcting those short comings and making it even better!
To accomplish that, we adopted a strategy for integrating discoveries in medicine, physics, and cognitive science to bridge the gap between the “explanation”…. The how and why something works and the “action”…we know that it works, now how do we apply it and make it better?


Ketamine Research Institute Scientific Presentation
“A New Methodological Approach to Improve the "Real World" Effectiveness of Ketamine Infusion Therapy for Treatment-Resistant Depression”
 We are excited to announce that our innovative approach to ketamine infusion therapy, utilizing precision medicine and target-controlled infusions, has been accepted for scientific presentation at the 2023 Annual Meeting of the American Psychiatric Association in San Francisco. Our methodological approach has been shown to significantly improve the "real world" effectiveness of ketamine infusion therapy for treatment-resistant depression, resulting in improved outcomes for patients. This acceptance is a testament to our approach's importance and potential impact, and we look forward to sharing our findings with fellow clinicians and researchers at this prestigious event.
We are excited to announce that our innovative approach to ketamine infusion therapy, utilizing precision medicine and target-controlled infusions, has been accepted for scientific presentation at the 2023 Annual Meeting of the American Psychiatric Association in San Francisco. Our methodological approach has been shown to significantly improve the "real world" effectiveness of ketamine infusion therapy for treatment-resistant depression, resulting in improved outcomes for patients. This acceptance is a testament to our approach's importance and potential impact, and we look forward to sharing our findings with fellow clinicians and researchers at this prestigious event.

RESTORE: A Precision Medicine and Systems/Network-Based Approach to Increase the Efficiency, Effectiveness, and Durability of the Standard Ketamine Infusion
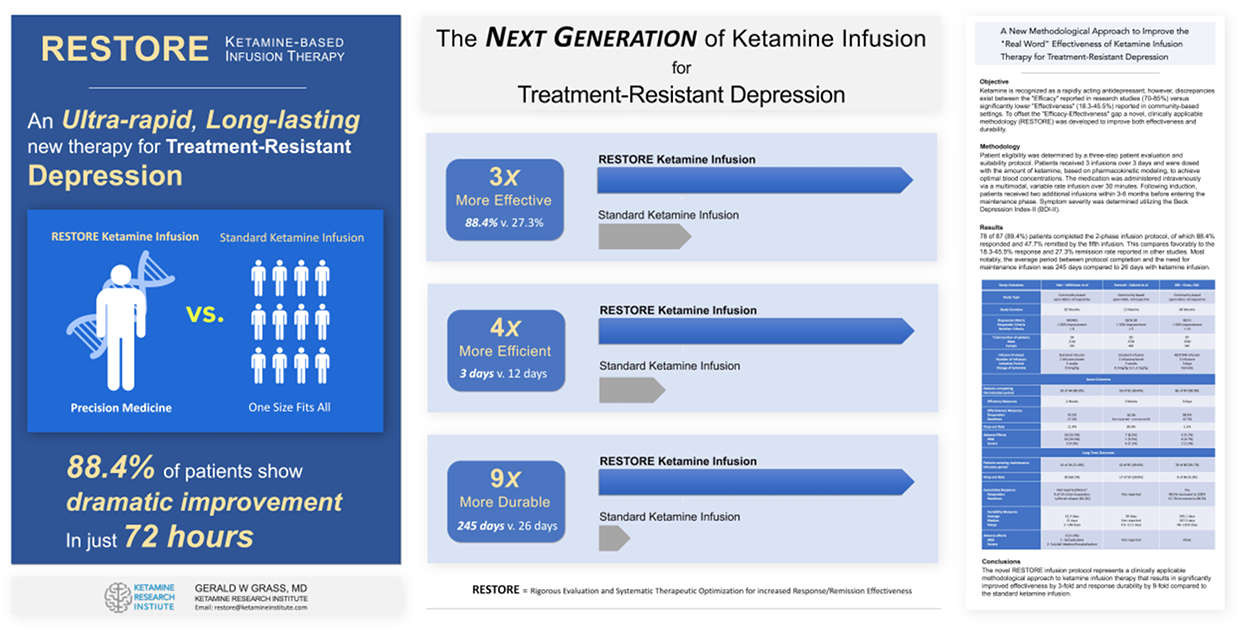
I adopted an alternative strategy for investigating ketamine based upon a Precision Medicine and "synergistic systems approach." This new emerging framework in research circles attempts to account for the actions of multiple variables jointly contributing to the therapeutic action of a drug.
It is an approach well suited to a drug with an established but only partially known therapeutic mechanism of action, such as ketamine. It incorporates strategies and methodologies to therapeutically "enhance" the drug's effect by eliminating or minimizing the impact of these variables. Moreover, it also employs augmentation strategies to systematically exploit the known interactions of the various components in the system in such a way as to maximize its overall efficacy.
After recognizing these issues as critical to the efficiency, effectiveness, and durability of ketamine infusion therapy, I have, for the past 20 years, endeavored to ascertain, evaluate, and catalog as many clinically relevant variables as possible that are reported or suspected to contribute to the pathogenesis of depression. My study of these variables also included those which may influence the effectiveness of ketamine based upon individual patient characteristics, such as individual body mass characteristics, metabolism, concurrent medications, pharmacogenomics, and psychological variables.
Anesthesiologists are familiar with many variables influencing drug metabolism, including volatile and intravenous anesthetic agents. In anesthesia research, a great deal of time is devoted to determining what is known as the minimum effective dose of an intravenously administered anesthetic agent required to produce a therapeutic response. The minimally effective dose (ED) is best defined as the dose of a drug needed to have the desired effect in 50%, 75%, or 95% of the patient population and is commonly expressed as ED50, ED75, and ED95 for that drug.
The first phase of my early research, which began in 2002, was primarily concerned with determining the effective dose, measured in nanograms/milliliter of blood, of ketamine necessary to achieve at least a 75% or better response rate in the typical patient population. Specifically, I was focused on determining the ED50, ED75, and ED95 of ketamine in my population of patients.
Prior research indicated that blood levels of 150 to 200 ng/mL were effective for approximately 50-70% of homogeneous groups of individuals participating in well-controlled trials. However, this did not necessarily translate to the general population of depressed patients seen clinically.
A second corollary question arose concerning the optimal concentration-time interval necessary to maintain a patient under the dose-response curve. It is important to recall that the 40-minute, constant rate infusion protocol used in the standard ketamine infusion was adopted somewhat arbitrarily and did not necessarily reflect adequate consideration of the pharmacologic principles used in intravenous anesthetic administration.
Therefore, it was essential to determine not only the ED50-ED95 of ketamine but also to evaluate the dosage of ketamine necessary and the optimal infusion sequence and rate of infusion necessary to exploit the balance between the given dose and selected method/rate of infusion versus the ability of the individual to metabolize and clear the drug from the body simultaneously. This relationship is known as the "area under the plasma concentration-time curve" or AUC.
The third unknown was related to the efficiency of ketamine therapy, or the “induction” period. Induction is the minimum number of sequential infusions necessary to be given over the shortest possible time interval to prolong the durability of the therapeutic response beyond 28 days. These were all critical questions that needed to be answered as they would have important implications for the standardization and clinical applicability of ketamine infusion therapy.
To address these issues, I performed numerous ketamine infusions over several years and carefully recorded and analyzed the results. Those observations led to the development of what was referred to, at that time, as an enhanced Multimodal Infusion Technique (eMIT). The technique optimized the effective minimum dose requirement of ketamine and prolonged the time under the dose-respond curve in such a way as to significantly improved the efficiency and effectiveness of the ketamine infusion. Its early success resulted in the submission and acceptance of a case report on applying this technique to the American Academy of Pain Medicine and the American Society of Regional Anesthesia Annual Meetings for presentation in 2016.
The second phase of my work from 2013 to the present has focused on three interrelated areas: first, accounting for the numerous factors known to contribute to the pathogenesis of depression and how one may minimize them before performing ketamine infusion therapy. Second, if it were not possible to eliminate them entirely, would it be possible to offset the impact of the various underlying metabolic, genetic, or medication-related effects on ketamine pharmacokinetic/pharmacodynamic (PK/PD) parameters in such a way as to achieve adequate blood concentrations. And finally, what augmentation strategies could be exploited, pharmacologically or psychologically, to enhance treatment effectiveness and durability.
The combined use of the eMIT infusion protocol and a Rigorous patient Evaluation and Systematic Therapeutic Optimization for increased Response/Remission Effectiveness strategy later became known as the RESTORE Infusion program.
The ultimate purpose of these investigations was to develop a ketamine infusion program incorporating a clinically applicable patient selection process, pre-infusion optimization strategy, and more pharmacologically advantageous infusion protocol to provide more effective treatment for patients with treatment-resistant depression than the standard ketamine infusion protocol.
Comparison of RESTORE to the Standard Ketamine Infusion -
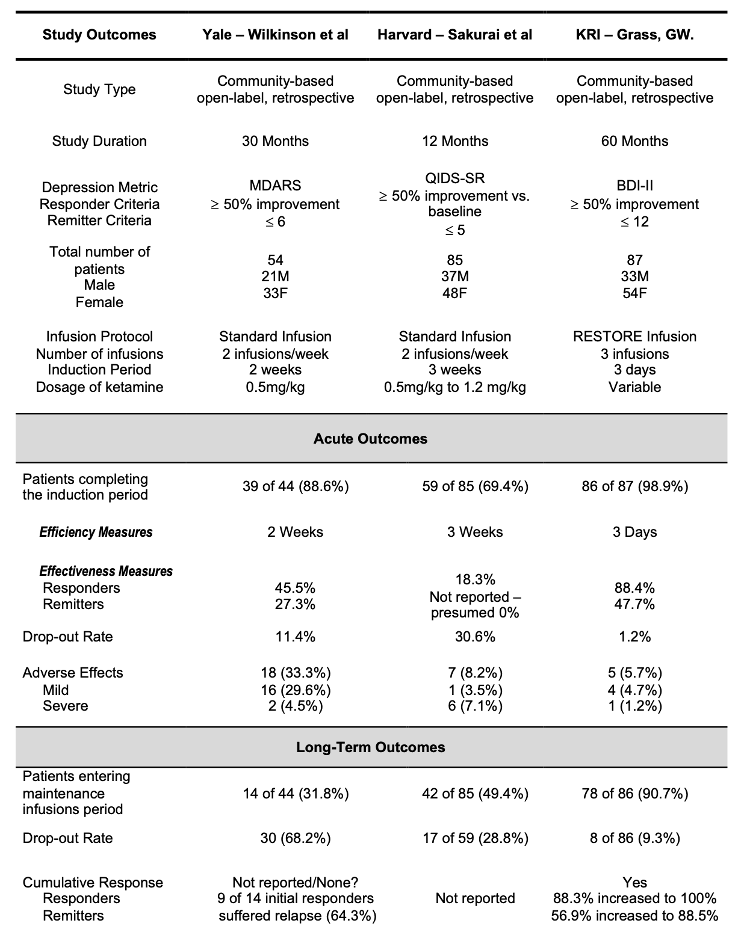
Conclusion:
RESTORE infusion program is: more rapidly acting (6-fold reduced induction time - Efficiency), more effective (3-fold Increase in Therapeutic Response - Effectiveness), and longer-lasting (9.4-Fold increase in Durability) when compared to the standard ketamine infusion for the safe and effective therapy for patients with treatment-resistant depression in private practice, community-based settings.
Educational Programs in Ketamine Infusion Therapy
For clinicians who want to learn more about a Precision Medicine and Target-Controlled Infusion approach to optimized ketamine therapy, the Ketamine Research Institute also offers an intensive and comprehensive training program in ketamine-based therapy. The training program provides the knowledge and skill set needed to achieve the same level of effectiveness demonstrated in high-level, well-controlled research studies and meets or exceeds the recommendations put forth by the American Psychiatric Association and the American Society of Anesthesiologists, including both a sophisticated didactic component and a supervised clinical administration of ketamine infusion therapy component.


The NEW Generation Of Ketamine Therapy...
The Restore Infusion

Request a Free Phone Consultation
Call - 800.850.6979
Consult with our experienced team to determine if Restore is right for you. Call us today or submit this request for a confidential consultation.
[contact-form-7 id="227" title="Untitled"]
